Pathophysiology of Kidney Tubular Injury and Chronic Fibrosis
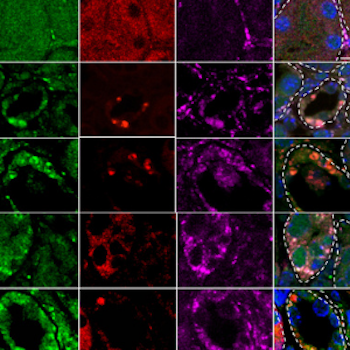
Pathophysiology of Kidney Tubular Injury and Chronic Fibrosis: A major focus of the laboratory has been the study of the pathophysiology of acute renal failure and processes involved with repair. There are many parallels between repair and the normal development of the kidney. While repair is generally considered to be adaptive it can be maladaptive, especially when the acute injury is superimposed on chronic kidney disease. Hence the large effort that has gone into understanding developmental systems will potentially translate into therapeutic approaches to treatment of adult as well as pediatric renal diseases. As a result of our experiments we have placed inflammation at the core of the pathophysiology and are continuing to explore the role of inflammation in the pathophysiology of acute renal injury and ways in which we can interrupt this response and reduce injury. We have found two proteins, KIM-1, an epithelial protein and nmb, a macrophage protein, which we believe play critical roles in the response of the kidney and have created a Kim-1 knockout/Gal4 knockin animal which will potentially allow us to use the characteristics of the promoter region of Kim-1 to express proteins specifically in the S3 segment of the proximal tubule, where most of the injury occurs. In addition, we want to understand the factors determining the recovery of the kidney in order to design strategies to enhance and hasten the processes necessary for recovery. These latter goals necessitate multiple experimental approaches. My laboratory carries out whole animal experiments on normal or knockout animals in order to test potential pharmacologic treatments or to test the hypothesis that a particular protein is important to the injury or repair process. More recently we have established models of preconditioning in the mouse in which we have uncoupled exposure to ischemia from the normal functional consequences of ischemia. We are employing genomic approaches to identify genes whose expression patterns might explain the profound protection we can induce in these models. We are using blood and urine proteomic approaches to identify new biomarkers and targets for therapy. Current studies have focused on genetic mouse models and zebrafish and include the role of stem cells in the repair process of the kidney post-ischemia.